The Paralysis of Analysis
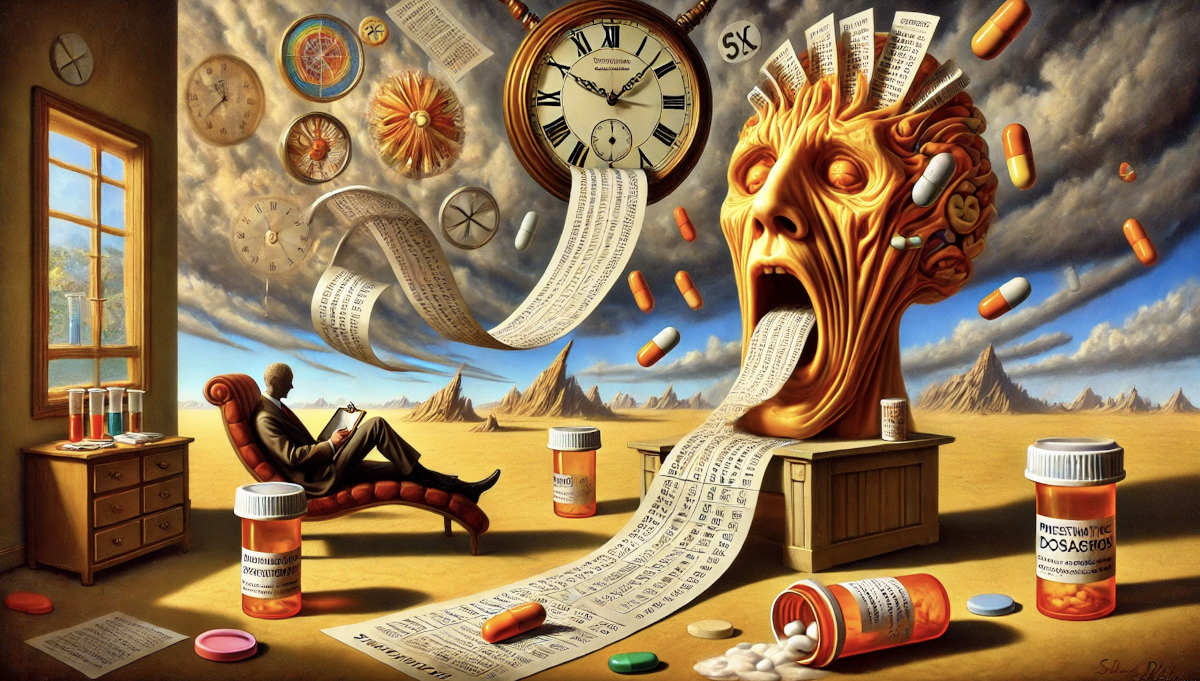
The Paralysis of Analysis: The Shortcomings of Psychological Assessments and the Global Mental Health Crisis
In the world of psychology, the assessment tools we rely upon serve as both guiding lights and shackles. We have developed intricate matrices, diagnostic criteria and algorithmic evaluations to understand the complexities of the human mind. However, there is an unsettling paradox at play. While these tools claim to offer clarity, they often over simplify the nuanced realities of human suffering. In many cases, they fail not only the individual but also the larger system of mental health care.
The Problem with Psychological Assessments
The modern psychological assessment industry is built upon standardised tests such as the Minnesota Multiphasic Personality Inventory (MMPI), the Beck Depression Inventory (BDI, and the Diagnostic and Statistical Manual of Mental Disorders (DSM–5). While these tools aim to provide structured insights into mental health, their limitations are glaring. They operate under the premise that human experiences can be neatly categorised into boxes, yet the fluidity of emotions and thought patterns defies such rigid classification.
-
Cultural Bias & Lack of Individualisation, Psychological assessments often fail to account for cultural variances. The DSM – 5, for instance is largely Westerncentric, imposing Euro – American frameworks onto diverse populations. A diagnosis of depression in an East Asian or African context, yet these differences are often disregarded.
-
Over-Reliance on Self-Reporting Many psychological assessments depend on self-reporting, which can be problematic. Clients may either exaggerate symptoms or underreport them due to stigma, lack of insight or personal biases. This means that conclusions drawn from such assessments are often incomplete or inaccurate.
-
Reductionist Approach Psychological assessment tools attempt to quantify the unquantifiable. They take dynamic, evolving human emotions and behaviours and reduce them to numbers, scores or diagnostic labels. A person’s pain, trauma or existential crisis cannot always be mapped onto a Likert scale.
-
Pathologising Normal Reactions The DSM-5 and similar assessment manuals increasingly medicalise normal emotional responses to life events. For instance the line between grief and clinical depression has been blurred, leading to overdiagnosis and subsequent overmedication.
The Overmedication Epidemic: The United States Leading the Tables
-
The limitations of psychological assessment tools have not only led to misdiagnoses but also fueled the global over prescription of psychotropic drugs. Nowhere is this issue more pronounced than in the United States, which has the highest rates of psychotropic drug prescriptions in the world.
-
In the US, over 23% of adults are on Psychiatric medication at any given time, with antidepressants and anti- anxiety medications being the most commonly prescribed.
-
The rates of ADHD diagnoses in children have skyrocketed, leading to a staggering 60% of diagnosed children being placed on stimulant medication.
-
Benzodiazepine prescriptions (e.g., Xanex, Valium) have surged, contributing to dependency and withdrawal crisis.
Contrast this with Europe, where mental health treatment still prioritises therapy over medication in many countries. France, Germany and the Netherlands place a stronger emphasis on psychodynamic therapy, cognitive – behavioural therapy (CBT) and holistic interventions.
Even more striking is the case of Japan, where mental Illness carries a significant stigma, resulting in far lower prescription rates. However, this also comes at a cost- many individuals suffer in silence due to a lack of accessible mental health care.
Little – Known Insights: The Politics of Psychiatry
-
The DSM-5 was heavily influenced by pharmaceutical companies. A significant amount of contributors to the manual, have financial ties to the pharmaceutical industry, leading to concerns that new disorders are added or broadened to expand the market for Psychiatric drugs.
-
Many psychological assessments are outdated. For example, the MMPI was developed in the 1940s, yet it remains one of the most widely used personality assessment tools despite cultural shifts and evolving psychological paradigms.
-
Placebo effects in psychotropic medication are more powerful than most realise. Studies have shown that for mild to moderate depression, placebos can be just as effective as antidepressants, raising concerns about the necessity of these medications for many patients.
-
Psychedelic therapies are challenging traditional psychiatric models. Psychedelics such as psilocybin (magic mushrooms), ketamine and MDMA are showing promise in treating treatment-resistant depression and PTSD, yet mainstream psychiatry has been slow to adopt them due to regulatory hurdles and industry interests.
-
Theoretical alternatives to traditional assessments exist but are often overlooked. Carl Jung’s concept of the shadow self, Maslow’s hierarchy of need and Viktor Frankl’s logotherapy, which emphasises meaning over pathology, provide richer more individualised approached to psychological assessment.
The Need for a Paradigm Shift
The future of mental health care must move beyond the mechanistic symptom focused approach of traditional psychological assessments and psychotropic interventions. Instead we should advocate for:
-
Holistic and Integrative Assessments – Incorporating methods such ad biofeedback neurifeedback heart rate variability analysis and energy psychology techniques into assessments for a more dynamic understanding of a person’s mental health.
-
A Return to Narrative Psychology – Moving away from rigid diagnoses and instead listening to an individual’s story, struggles and personal context to guide treatment.
-
Global Mental Health Reform – Encouraging more personalised, culturally sensitive approached rather than imposing Western diagnostic models onto diverse populations.
-
Reduced Dependency on Psychotropic Medication – Encouraging therapy first approached mindfulness and alternative treatments before resorting to psychiatric drugs.
-
Greater Transparency in the Psychiatry-Pharmaceutical Relationship. A push for less pharmaceutical influence over mental health policies and diagnostic criteria.
“ When a measure becomes a target, it ceases to be a good measure.” Goodhart’s Law
Final Thoughts
Psychology has long been revered as the study of the human soul, yet modern mental health assessment tools often reduce individuals to more checklists of symptoms. This paralysis of analysis where excessive reliance on outdated, flawed psychological assessments leads to overdiagnosis, overmedication and oversimplification must be challenged.
As the Founder of www.psychologistics.org, I advocate for a more human centred approach, one that prioritises individual narratives holistic healing and critical inquiry into the methodologies that govern mental health care today. If we truly wish to serve those in distress, we must step beyond the constraints of rigid diagnostics and reclaim the soul of psychology.
